Take the last step in your Revenue Cycle
Causes & Effects of Swelling
Patient Financial Responsibility
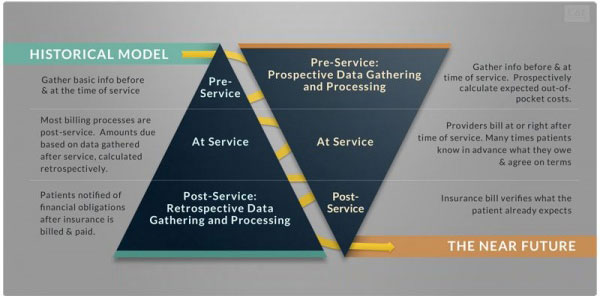
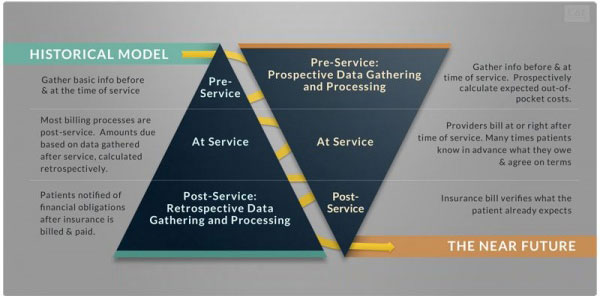
The pace of change in the healthcare industry is accelerating rapidly. Higher expectations by patients for quality, cost, and transparency reflect our consumer-centric economy.
One of the most significant changes impacting healthcare providers is the shift from third-party payers to patient responsibility…
Learn More ›
Traditional Revenue Cycle
Processes No Longer Work
Increased patient responsibility is squeezing providers’ revenues and margins. The vast majority of patients are willing to pay what they owe but they also expect to get clear cost estimates up-front and flexible payment options.
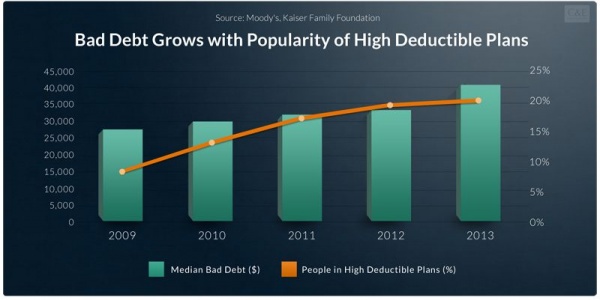
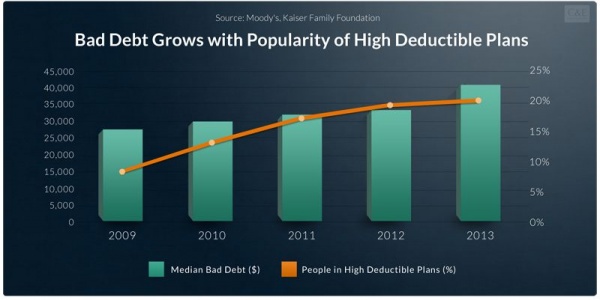
Ballooning subscriptions to HDHPs magnify the importance and urgency of verifying patients’ eligibility, estimating patients’ out-of-pockets costs…
Learn More ›
Read The Latest Posts From Our Blog: C&E Perspectives
One of the primary responsibilities of a hospital executive, is the protection and management of all hospital assets. This means implementing processes to monitor and maintain the ability of every asset to support the hospital’s mission.
There’s been a major shift in the mix of healthcare payers due to the growth in high-deductible health plans and to increases in employee cost-sharing of employer-sponsored plans. As more people accept responsibility for more of their healthcare expenses, hospitals must collect more money from more payers who have more accounts with hospitals and affiliates…. Read more »
Healthcare CFOs have a lot of things to think about right now. From keeping up with the latest technological trends to maintaining relationships between physicians and hospitals, it is likely your schedule is already full. Therefore, the last thing you need is to worry about patient medical debt. Let’s take a look at what healthcare CFOs should and should not have as their top concerns.